Key takeaways
The UK government’s recent NHS 10 year plan imagines a health service free of manual processes, long patient wait times, and burnt out staff. To reach this equilibrium, practices and trusts must rethink their current processes and commit to extensive digital transformation. In this blog, we dissect the key mission statements in the 10 year NHS plan, identify 6 digital transformation priorities, and help you navigate any risks or objections.

A secure foundation for NHS digital transformation
In the summer of 2025, the UK government unveiled a 10 year plan for NHS England, titled “Fit for the Future”. This plan details a wave of anticipated changes, from adapting the NHS operating model to boosting staff morale and reducing patient wait times.
The biggest takeaway from the document, however, is the government’s resolute commitment to digital transformation.
In this blog, we’ll summarize the key mission statements of the plan, extract 6 critical digital transformation priorities, and help you mitigate any risks or objections.
The NHS 10 year plan: A brief overview
“The choice for the NHS is stark: reform or die.”
These words from the government’s executive summary paint the picture well. In its current state, the NHS is unsustainable. The majority of patients struggle to book GP appointments. Wait times are astronomical. And burnout seems to be part and parcel of the staff experience.
This is why the government has drafted a revolutionary 10 year plan; not to overstretch the NHS, but to save it.
The document is well over 100 pages long and contains 9 core mission statements:
- “It’s change or bust: We choose change”. Change is fundamental for the NHS’s survival, but it’s also a key opportunity. The NHS has an unprecedented level of data at its disposal. As a single-payer system that treats patients from “cradle to grave”, it’s a prime candidate for digital transformation, predictive analytics, and genomics.
- “From hospital to community: The Neighbourhood Health Service designed around you”. Making the NHS more community focused, with an emphasis on elevating primary care, easing GP workloads, integrating new local healthcare centers, and streamlining patient triage with digital services.
- “From analogue to digital: Power in your hands”. Embracing AI to ease administrative work, enforcing NHS-wide app accessibility, and moving to a Single Patient Record (SPR) model.
- “From sickness to prevention: Power to make the healthy choice”. Increasing the health of UK citizens via healthy eating initiatives, vaping restrictions, health screenings, and early-detection tests.
- “A devolved and diverse NHS: A new operating model”. Decentralizing power from Whitehall and distributing it across local centers, providers, and patients.
- “A new transparency of quality of care”. Increasing standards of patient care, reducing instances of neglect, and creating a more accountable care model, supported by patient feedback.
- “An NHS workforce fit for the future”. Enabling NHS workers through focused, tailored training plans, healthier working environments, and flexible working options.
- “Powering transformation: Innovation to drive healthcare reform”. Pushing investments in AI, data interoperability, genomics and predictive analytics, robotics, and wearable technology. All in an effort to augment staff and improve patient outcomes.
- “Productivity and a new financial foundation”. Ensuring the NHS’s future is sustainable with fairer funding distribution, cuts to low-value spending, and new approaches to financial management.
Even from a top level perspective, the emphasis on digital transformation is plain to see. If everything goes according to the government’s vision, the future of the NHS will be paperless, automated, and in the palm of every patients’ hand.
To reach this digitally enabled state within 10 years, NHS teams will have to undergo extensive change.
From the outset, this may seem overwhelming. But we’re here to break it down into manageable steps.
In the following section of this article, we’ll list 6 key digital transformation priorities for your NHS organization, based on the guidance given in the government’s “Fit for the Future” plan.
6 digital transformation priorities for NHS trusts
1. Move beyond analogue processes
Paper records, manual processes, and telephone-based appointment bookings are still prevalent across NHS practices in England. These analogue processes don’t just impede patient experiences — they exacerbate the NHS’s well-documented productivity and burnout issues. It’s a lose-lose for everyone involved.
The government wishes to eradicate these analogue bottlenecks and replace them with NHS Online services; one application where patients can book appointments, manage prescriptions, and discuss health concerns with clinicians in real time.
To make this a reality across NHS England, organizations will need to:
- Build online appointment booking forms and patient self-referal services
- Test online services in regards to usability and accessibility
- Finely tune clinician workflows to ensure no requests fall through the cracks
- Train staff on new systems and provide educational resources for patients who may lack technological confidence
Practices must also work towards digitizing their current paper-based processes. Storing records in a secure, version-controlled document management system — available to all appropriate personnel — will encourage greater accessibility and knowledge sharing. All while reducing the frustration of searching through reams of storage cabinets to find the right document for the right patient or procedure.
2. Improve data interoperability
Data interoperability is an emerging priority across global healthcare organizations. In short, it refers to the seamless exchange of health data between systems — both internally and externally. This allows organizations to obtain a more complete picture of individual patient health, as well as increase the value of their extensive data sets.
As the 10 year NHS plan succinctly puts it, “high-quality, interoperable health data is the lifeblood for AI algorithms.” But it’s also key to accommodating another item on the government’s wishlist: to deploy UK-registered professionals in other countries and provide 24/7 access to patients.
Data interoperability will be essential for maintaining these relationships, as organizations can only collaborate with standardized data.
Improving interoperability will require a handful of steps:
- Digitizing records and ensuring consistency across data sets
- Adopting uniform data standards, such as the HL7 Fast Healthcare Interoperability Resources (FHIR)
- Integrating digital tools and platforms via API
- Ensuring data governance and bolstering data security across data points
For more information on data interoperability in healthcare, read our dedicated blog.
3. Give patients a single point of access to their data
This brings us onto a related digital transformation priority: the “Single Patient Record” (SPR). Taking inspiration from similar healthcare innovations in Australia and Estonia, the SPR is a living, digitized patient profile that unifies a wealth of medical data. This includes past appointments, observation notes, prescription details, patient vitals, and even data from wearable devices. Clinicians and patients can log into this record at any time and add data whenever necessary.
Data interoperability is the foundation of this unified record. Unless data can seamlessly move between systems and devices, the SPR simply won’t work.
However, that’s not the only challenge NHS organizations will have to contend with. Creating a centralized, digital location for this data is equally as important.
The SPR must be remotely accessible, easy to navigate, and compliant. This requires an intuitive platform with extranet features and granular user permissions. That way, you can permit access rights to external partners, relevant global providers, and patients — all without compromising data security.
4. Automate administrative tasks
By automating administrative tasks, practices can improve time to care rates, alleviate employee stress, and better prepare for future staff shortages.
However, there’s no one-size-fits-all use case for automation. That’s why it’s crucial to assess your current inefficiencies and identify quick wins for your organization specifically.
Many of our healthcare customers harness our process automation tool, InfoCapture, for digitizing internal processes, such as employee performance reviews, incident/accident reports, and compliance procedures. But the possibilities are almost endless.
For example, the government’s 10 year plan highlights the potential of automated data reports. One clinically led collaboration in England currently integrates patient health information from surgical waiting lists and primary care records. The resulting RAIDR dashboard eliminates manual information searching and analysis. Clinicians and anesthetics can get a clear overview of patient health — and provide personalized treatment plans/medication to improve their condition — before their surgical procedure takes place.
5. Augment staff with the help of AI
While almost 50% of US healthcare organizations already implement AI in their operations, the UK is lagging behind. This is soon set to change.
For 5 years, NHS England’s dedicated AI team have been documenting AI use cases, development best practices, and research. Now, the government is keen to scale the success of these initial trials across practices and hospitals.
In the 10 year NHS plan, they specifically call out “ambient AI”. This technology listens into conversations during patient appointments and makes a note of important information in the relevant care record. In turn, reducing the need to take notes and improving the overall patient experience.
But the potential of AI technologies stretches far beyond this. For example, intelligent AI assistants can help clinicians — and even patients — better understand complex research documents, treatment plans, and policies. By improving contextual understanding, clinicians can make decisions faster and patients can feel more assured about their care.
6. Provide digital and personalized training plans
The UK government is planning a complete NHS workforce reform. Training is fundamental to this.
In chapter 7 of the plan, they reference digital skills training, mandatory training reform, and “skill escalator” pathways. In short, the government plans to eradicate repetitive training and enable clinicians with clear, tailored development roadmaps. They boldly claim: “By 2035, every single member of NHS staff will have their own personalised career coaching and development plan, to help them acquire new skills and practice at the top of their professional capability.”
To bring this to life, NHS leaders must harness training platforms that encourage personalized learning pathway creation, automated certification and tracking, and integration with in-person courses and events. The more scalable these platforms, the better — especially for larger Trusts or NHS collaborations.

Revolutionize NHS operations
Digitize analogue processes.
Upskill your workforce.
Centralize your data.

Overcoming the 3 biggest barriers of digital innovation in healthcare
The government’s “Fit for the Future” plan is intentionally positive. But it’s important not to skim over the risks and barriers of sweeping digital innovation.
The NHS as a whole, as well as individual points of care, must carefully consider the following:
1. Data security
Data interoperability efforts, AI technologies, and SPRs will naturally increase the number of people and systems accessing sensitive healthcare data. This is a significant security and compliance risk — particularly for an industry that’s already a prime target for cybercriminals.
NHS organizations must actively protect patient data at every touch point. Encryption, granular user permissions, and IP-based access controls will ensure data is only accessible to those who have a right to access it. Secure AI tools (that don’t use your data for training purposes) will eradicate the possibility of data slipping out of your hands. And enforced, trackable e-learning courses centered around data protection will enable your clinicians to harness new technologies without putting patients at risk.
2. Change management
Implementing sweeping digital transformations isn’t as simple as flicking on a light switch. Change takes time to adjust to. For a workforce that’s severely burnt out, adding another task or tool could be the difference between an employee staying or going.
As a result, NHS England must roll out automation, AI, and any other digitization initiatives steadily. Projects should start small and then branch out. Leaders must demonstrate the positives while being mindful to check in and ask staff for feedback. And training should be bitesize, unobtrusive, and accessible.
The decade-long plan can only demonstrate ROI if everyone buys into it. So don’t just focus on the technologies and systems needed to deliver change; focus on the people it impacts, too.
3. Patient concerns
Patients will also require support to adapt to new digital services — especially if they have accessibility needs or lack experience with technology.
In a similar vein, NHS practices must also anticipate and mitigate any concerns surrounding AI. A recent study found that patients only support the use of AI if staff check the output afterwards. In particular, patients are vehemently against the use of unchecked AI outputs that support diagnoses and inform treatment plans.
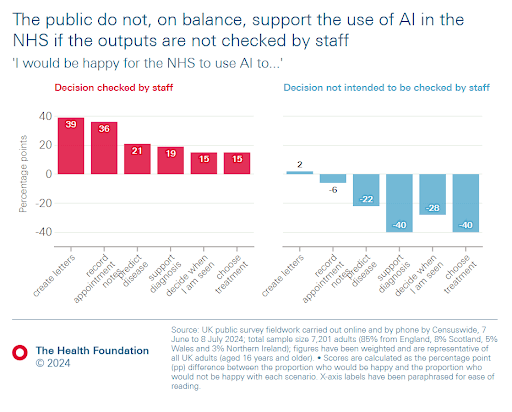
Image courtesy of The Health Foundation.
Though AI and automation can enhance patient outcomes, they may also become a cause of stress or concern. As a result, it’s important to balance convenience with quality.
Step into a better, brighter future with Claromentis
10 years may seem like a long time, but it’ll pass in the blink of an eye. NHS organizations in England must dismantle their outdated and unreliable paper processes, rethink their disparate tech stacks, and start planning for transformation now. All while firefighting current burnout challenges, growing patient demand, and ever-tightening data protection obligations.
This is no small feat. But the NHS needn’t bear the brunt of these transformation efforts alone.
Finding the right technology — and vendor — will help you turn ideas into actions, and actions into tangible results.
At Claromentis, our highly secure digital workplace solution can provide a foundation for this digital transformation. Comprising an AI-powered intranet, a no-code automation tool, and a SCORM-compliant learning management system, our solution helps you digitize your analogue processes, upskill your workforce, and centralize your data. Built-in security controls and granular user permissions ensure your PHI stays safe, while integration capabilities enable seamless data sharing.
To find out how we could revolutionize your healthcare operations, book a no-obligation discussion call with one of our experts. We’ll listen to your priorities, show you Claromentis’ capabilities, and plan a personalized package around your budget.
NHS 10 year plan FAQs
What are the key points of the NHS 10 year plan?
The NHS 10 year plan contains 9 key chapters — including the introduction — which all focus on a separate operational priority. The key highlights of the document include:
- Digitizing analogue and paper-based processes
- Adopting AI, genomics, and automation to streamline clinician workflows and improve patient outcomes
- Building a “neighborhood” health service, with an emphasis on strengthening community services and access
- Focusing on preventing illnesses rather than simply treating them
- Providing patients with 24/7 NHS Online services
- Improving resilience and skills across the NHS workforce, with every staff member receiving a personalized training plan by 2035
What are the three shifts in the NHS 10 year plan?
The NHS 10 year plan focuses on three shifts; “from hospital to community”; “from analogue to digital”; and “from sickness to prevention”.
- From hospital to community. This entails building a “neighborhood” health service, whereby people can receive treatment via local centers, clinics, pharmacies, an accessible mobile application, and within the home. The government’s aim is to increase the accessibility and reliability of healthcare services, as well as reduce complexity for patients currently navigating fragmented NHS systems.
- From analogue to digital. This mission statement involves the automation of manual processes, integration of ambient AI, and a focus on digitally-led healthcare services — all in a bid to augment healthcare staff and improve patient experiences. The government also wishes to introduce centralized “Single Patient Records” (SPR) for every patient.
- From sickness to prevention. A collaboration between the NHS and the UK government will aim to prevent illnesses through healthy eating initiatives, greater smoking and vaping restrictions, health and genomic testing, and innovative early-detection tests.
Who is leading the NHS 10 year plan?
The Department of Health and Social Care is leading the NHS 10 year “Fit for the Future” plan, with the assistance of NHS England’s CEO, Jim Mackey, and various experts across the NHS, UK government, and the Royal College of Nursing.
What are the NHS priorities for 2025?
NHS prioritises for 2025, leading into 2026, include:
- Reducing wait times for elective care, with every trust expected to improve by a minimum of 5%.
- Shortening A&E wait times to 4 hours for 78%+ patients, and ambulance response times to 30 minutes.
- Improving patient access to GPs and urgent dental care.
- Enhancing mental health services and pathways for adults and children alike, as well as reducing average length of stay in adult acute beds.

Step into the future of the NHS
Seamless, secure data sharing that helps you provide better patient care.

.jpg?width=1600&height=1000&name=artur-tumasjan-qLzWvcQq-V8-unsplash%20(1).jpg)


.jpg?width=400&height=250&name=vitaly-gariev-xDNwySMfR5I-unsplash%20(1).jpg)


.jpg?width=400&height=250&name=accuray-5VkNa1LrS8A-unsplash%20(1).jpg)